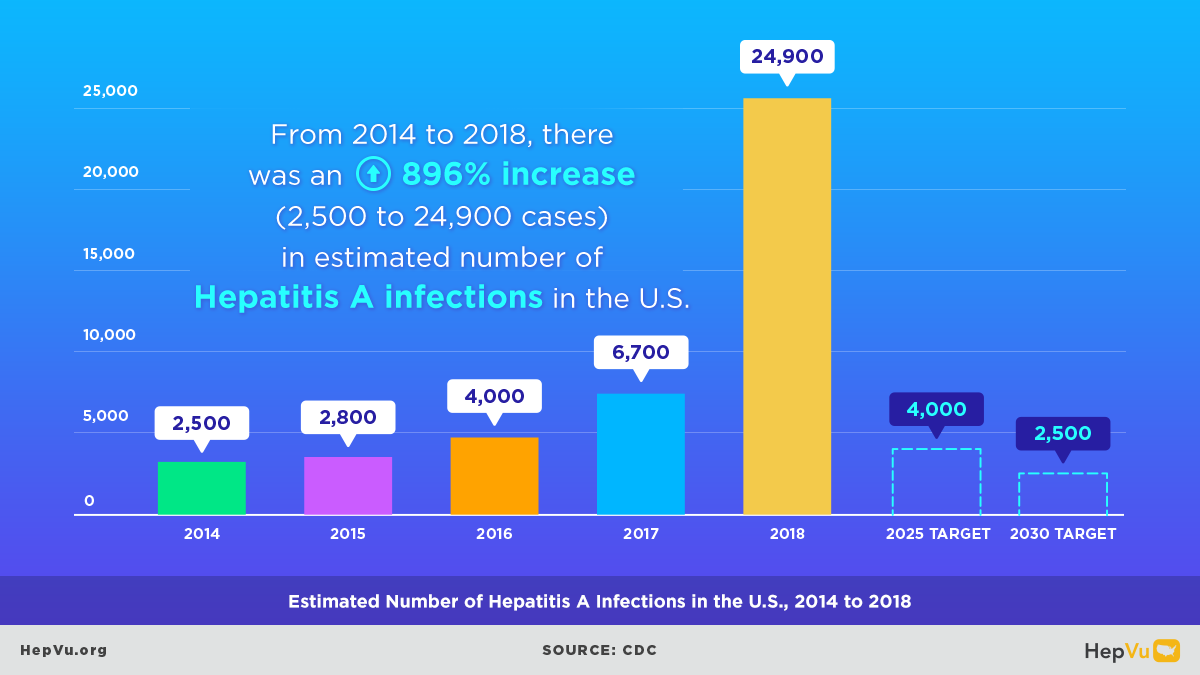
Millions of people in the United States are living with viral hepatitis. Chronic Hepatitis B affects an estimated 1–2 million Americans, and Hepatitis C affects approximately 4 million. While Hepatitis A outbreaks have declined in recent years due to expanded vaccination efforts, Hepatitis B and C persist – driven by the opioid crisis, gaps in routine screening and treatment, and persistent structural barriers. Health disparities remain stark, disproportionately affecting people who inject drugs, as well as Black, Hispanic/Latino, Asian and Pacific Islander, and American Indian and Alaska Native communities.
According to the World Health Organization (WHO), viral hepatitis elimination is defined as a 90% reduction in new infections and a 65% reduction in hepatitis-related deaths. In its 2016 agenda, the WHO set their goals to achieve viral hepatitis elimination by 2030. Highlighting the dangers of viral hepatitis and its negative effects that can lead to other diseases such as liver cancer, the WHO strongly recommended countries develop their own national elimination plans.
Federal Leadership and Changing Policy
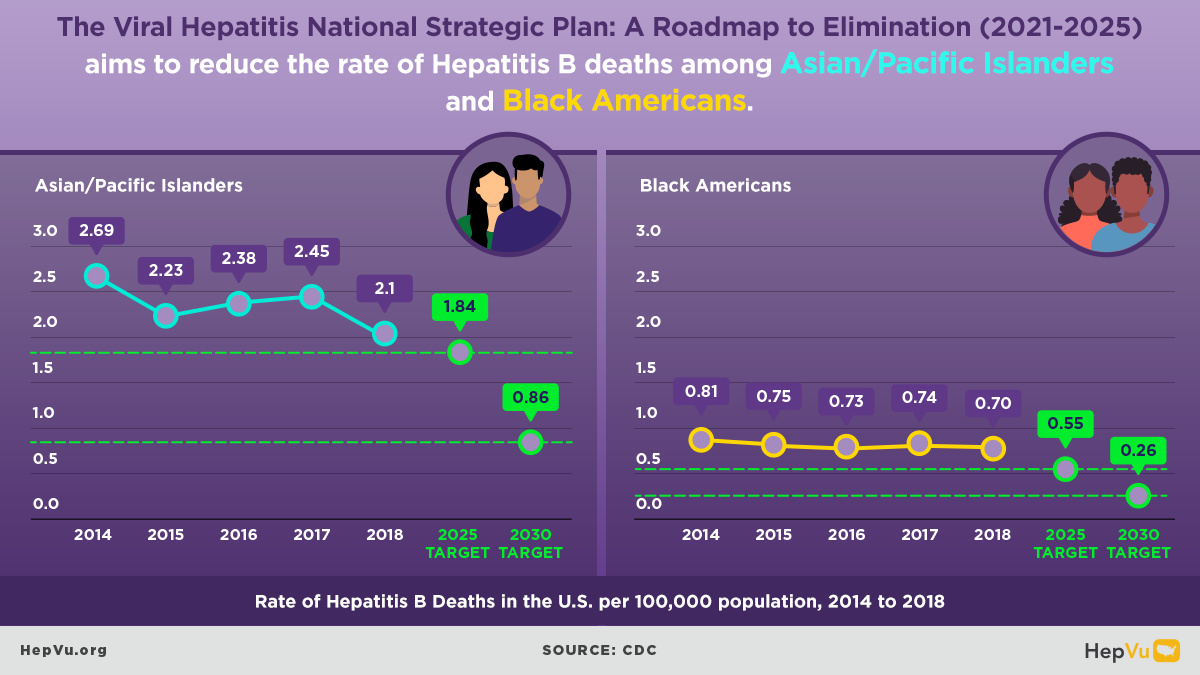
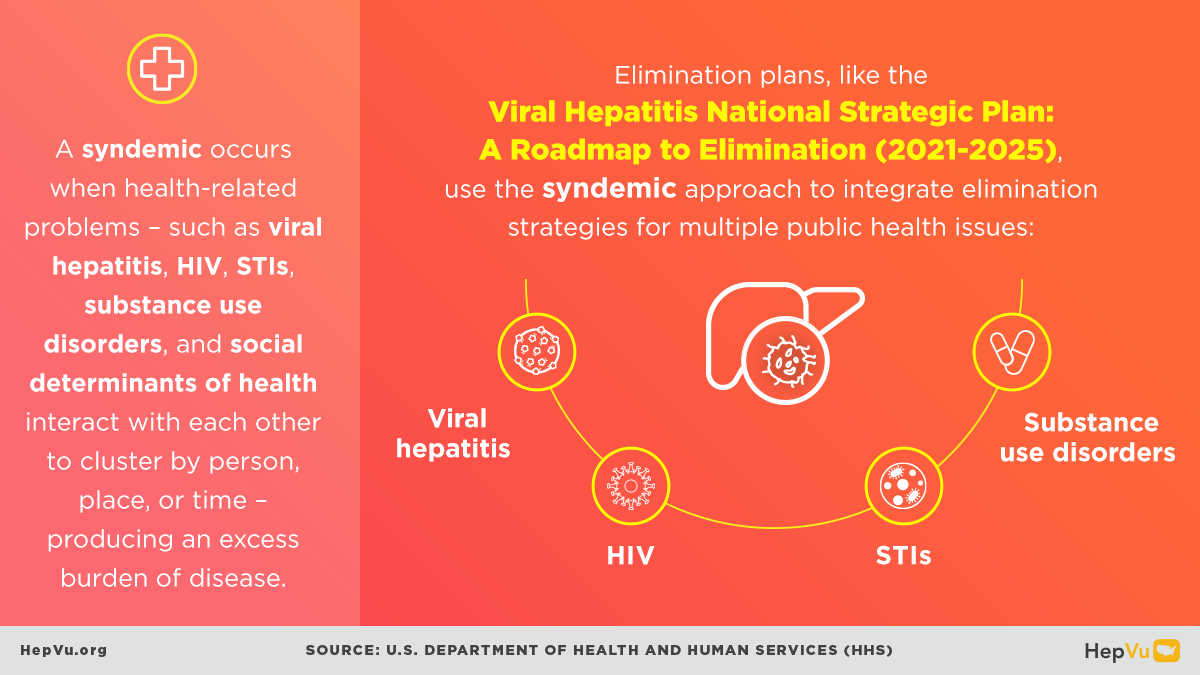
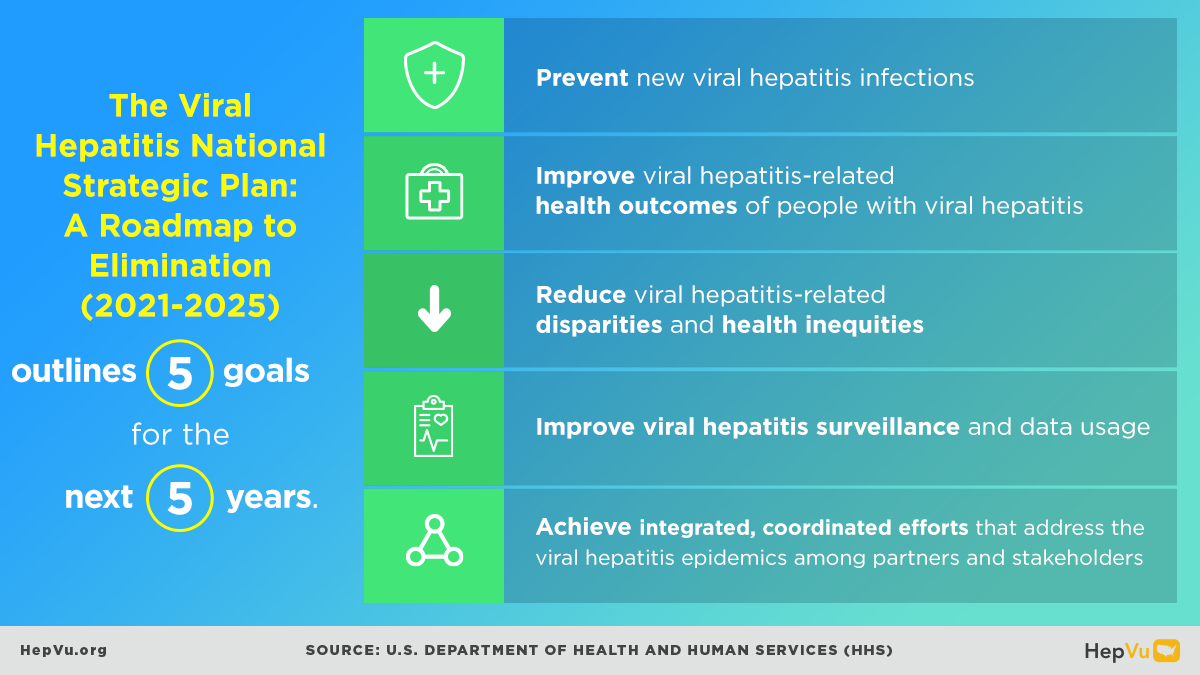
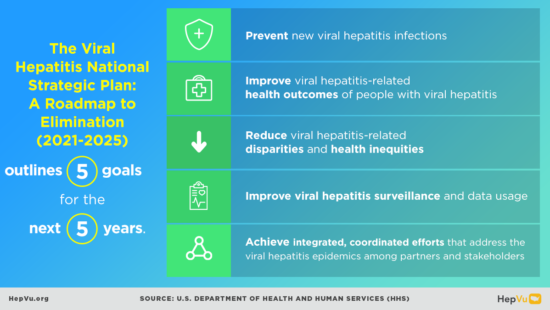
In January 2021, the U.S. Department of Health and Human Services (HHS) released the Viral Hepatitis National Strategic Plan: A Roadmap to Elimination 2021–2025. This framework identified shared objectives for researchers, policymakers, health providers, advocates, and communities to work collaboratively toward eliminating viral hepatitis as a public health threat.
The HHS plan prioritizes preventing new infections, improving outcomes for those living with hepatitis, reducing inequities, strengthening surveillance, and fostering partnership across sectors and levels of government. Notably, in 2022, CDC recommended universal Hepatitis B vaccination for adults ages 19–59, as well as one-time Hepatitis C screening for all adults and during every pregnancy to promote early detection and care linkage. In 2023, CDC further recommended that all adults be screened at least once for Hepatitis B infection.
The plan also emphasizes reducing disparities and inequities linked to social determinants of health, particularly among priority populations. These inequities contribute to missed opportunities for vaccination and screening, provider limitations, and inconsistent data collection. While the strategy outlines clear national objectives, it also underscores the importance of state and local leaders tailoring elimination efforts to meet community-specific needs, ensuring that strategies remain inclusive and equitable.
In 2023, former NIH Director Dr. Francis Collins called for a national strategy to eliminate hepatitis in the United States. for ending Hepatitis C reached a turning point in 2025, with bipartisan support for the Cure Hepatitis C Act (S.1941). Modeled after successful state-level pilots, the Act would:
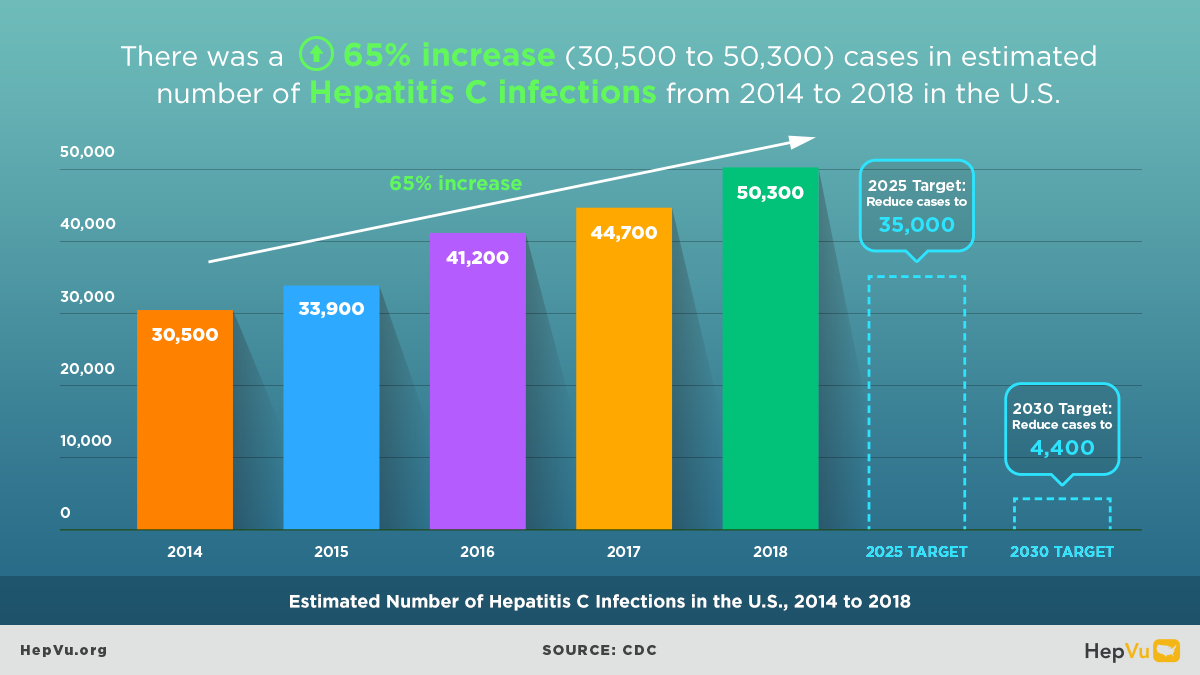
- Create a national Hepatitis C Elimination Program under HHS, investing nearly $10 billion through 2031 to expand rapid screening, diagnosis, and curative treatment, particularly for Medicaid recipients, uninsured or incarcerated individuals, and patients served by the Indian Health Service.
- Establish a subscription purchasing model through which the federal government would negotiate large-scale acquisitions of curative Hepatitis C medications, removing prior authorization barriers and expanding access in high-need areas.
- Waive cost-sharing for Medicare beneficiaries, improving affordability for older adults and people with disabilities.
- Provide funding to states and local jurisdictions to scale up outreach, testing, infrastructure, and data systems focused on high-burden communities.
- Set clear national goals, metrics, and advisory structures to track progress and ensure
Estimates suggest that curing Hepatitis C at scale could save more than $6 billion in federal spending over the next decade and prevent tens of thousands of deaths from liver disease.
CDC’s Division of Viral Hepatitis 2025 Strategic Plan
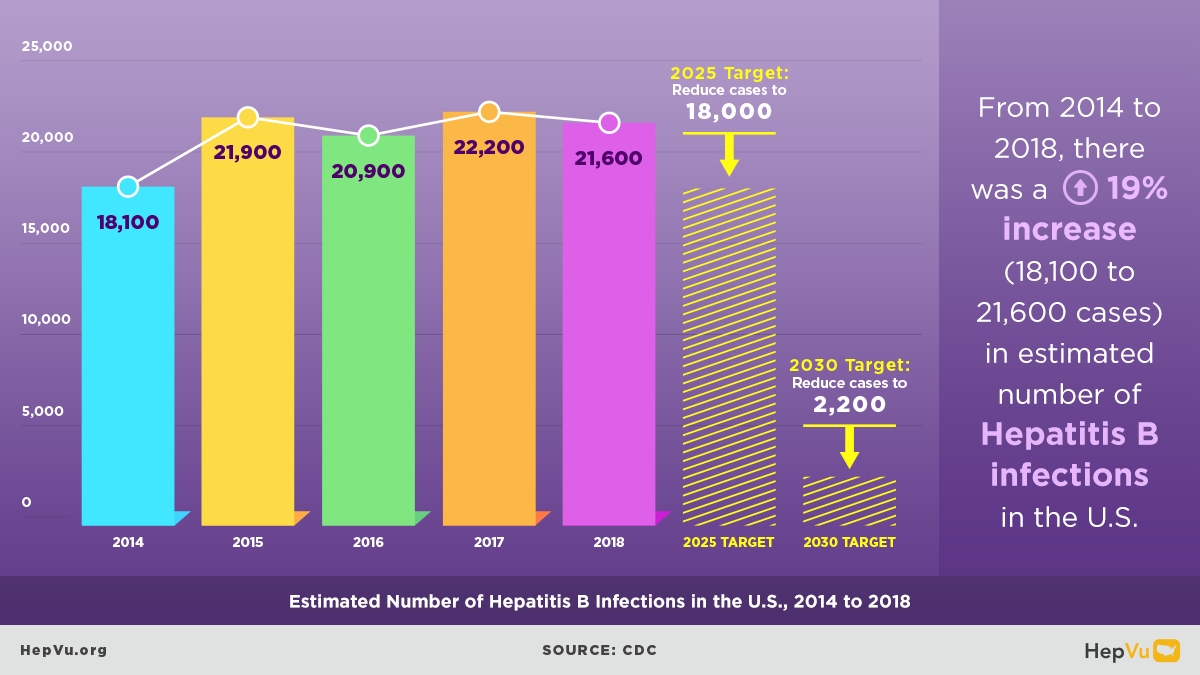
In September 2020, the CDC’s Division of Viral Hepatitis (DVH) released its 2025 Strategic Plan. The plan focuses on:
- Reducing viral hepatitis infections
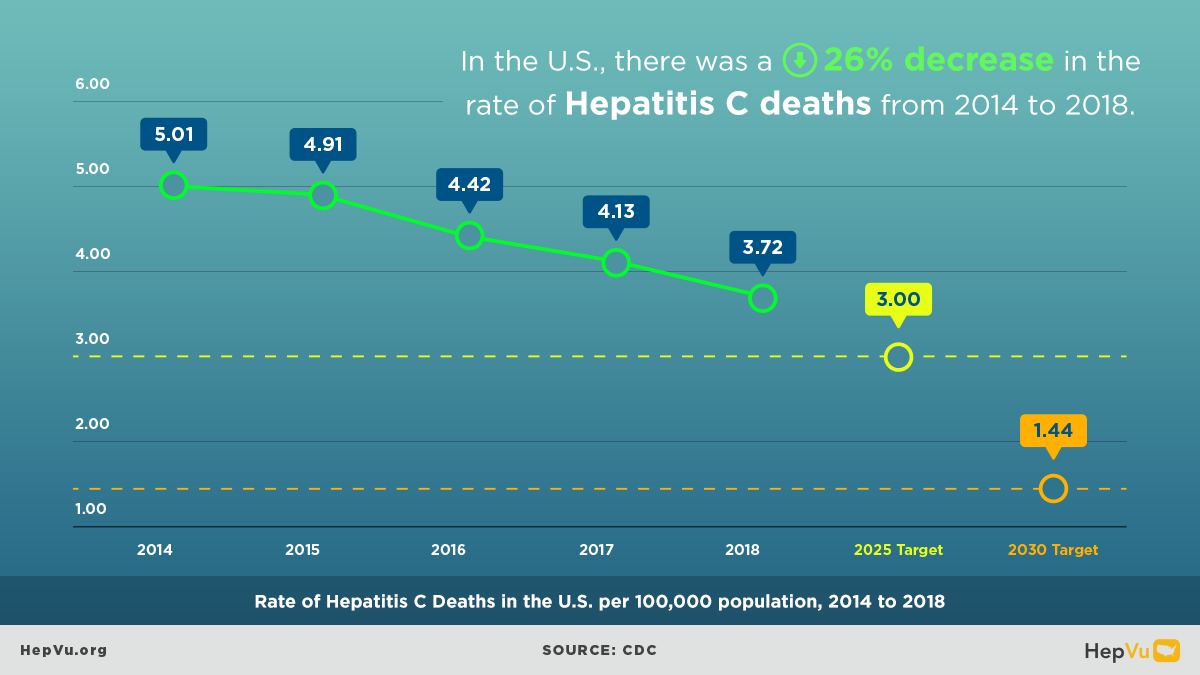
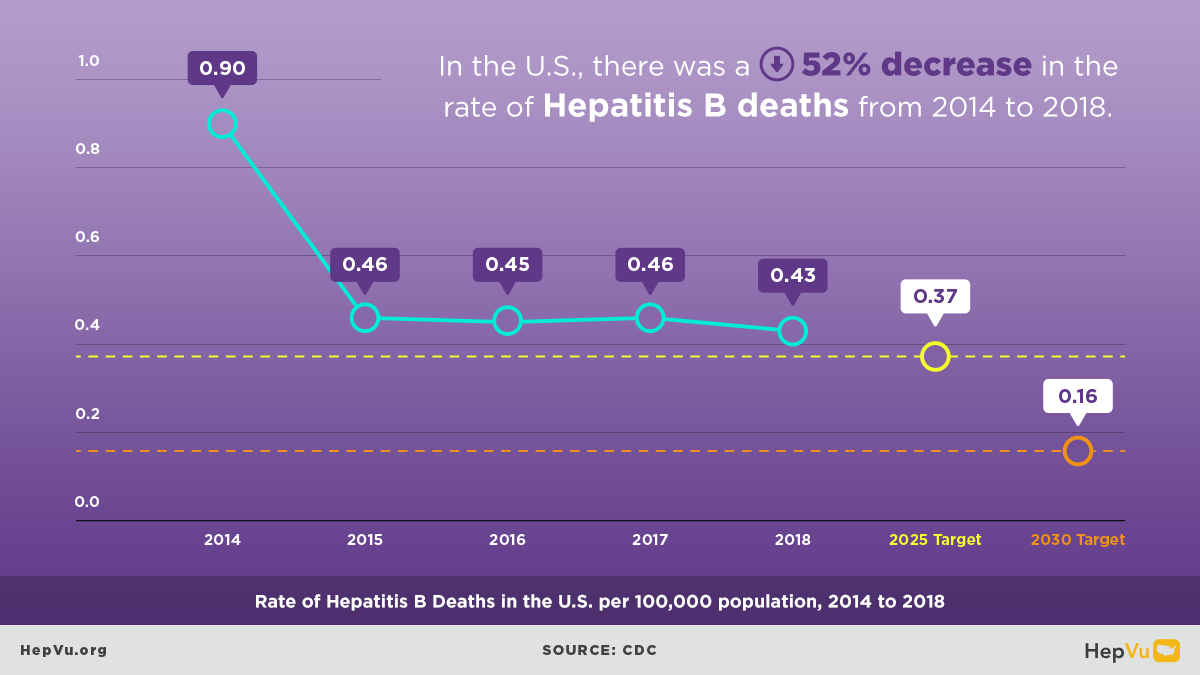
- Reducing viral hepatitis-related morbidity and mortality
- Reducing disparities in outcomes
- Establishing comprehensive national viral hepatitis surveillance
The DVH plan accelerates efforts to eliminate Hepatitis B and C as public health threats by 2030. Its priorities include scaling up universal Hepatitis B testing and vaccination for adults 19–59, expanding universal Hepatitis C screening for all adults and during every pregnancy, and addressing persistent inequities among disproportionately affected groups such as Black, Hispanic/Latine, Asian American and Pacific Islander, American Indian and Alaska Native populations, people who inject drugs, and justice-involved populations.
Aligned with the HHS strategy, the CDC DVH plan builds partnerships at the federal, state, and local levels and emphasizes improved data surveillance and equity-centered implementation. Developed with the global public health goal of eliminating viral hepatitis by 2030 in mind, the CDC DVH plan focuses on the next five years as a critical period in viral hepatitis elimination in the U.S.
Local Viral Hepatitis Elimination Plans
Across the country, states, cities, and tribal governments are advancing local viral hepatitis elimination strategies that respond to community needs. Examples include Hawaii’s Hep Free 2030, Washington State’s Hep C Free plan, Louisiana’s elimination initiative, and innovative models in California, New York, and Philadelphia.
These local efforts expand Hepatitis B testing and vaccination, integrate Hepatitis C screening and linkage to care in diverse settings (including corrections, primary care, and substance use treatment programs), reduce perinatal transmission, and address social and structural determinants of health. Many adopt a microelimination model – targeting high-risk populations such as people who inject drugs, justice-involved individuals, and people living with HIV – to achieve rapid, measurable progress through equity-driven, community-based strategies.
Microelimination
Microelimination refers to targeted efforts to eliminate Hepatitis C within specific populations or settings. By focusing on defined high-risk groups—such as people who inject drugs, individuals in correctional facilities, Tribal nations, and people living with HIV—microelimination initiatives have achieved notable gains in screening, care linkage, and treatment completion rates.
Correctional health programs have pioneered universal opt-out screening and direct-acting antiviral (DAA) treatment within facilities, reducing prevalence and reinfection. Tribal nations have leveraged sovereignty and community health systems to embed Hepatitis C care within culturally grounded wellness programs. Among people living with HIV and those who inject drugs, integrated care models effectively address co-infections, substance use, and treatment barriers.
These high-impact initiatives have informed federal and state policies, including key provisions of the Cure Hepatitis C Act. By scaling data-driven interventions, improving access to curative therapies, and prioritizing disproportionately affected populations, microelimination demonstrates that national elimination is achievable through focused investment, collaboration, and equitable design.
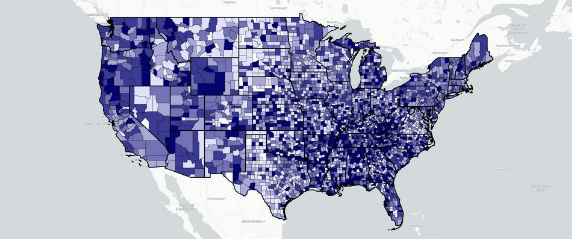
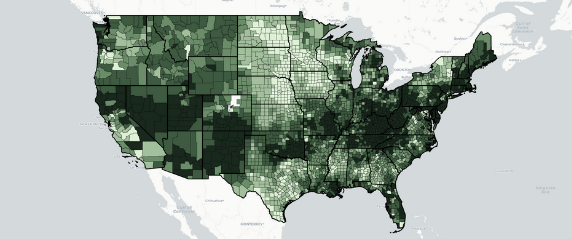
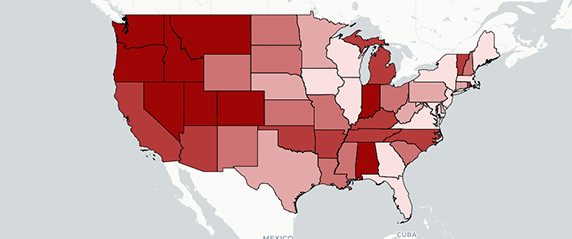
Surveillance
Surveillance data remain essential to achieving elimination goals. Accurate, timely, and comprehensive data help federal, state, and local partners identify gaps, direct resources, and measure progress. Ongoing federal strategies are modernizing hepatitis surveillance infrastructure, enabling more robust local data, targeted outreach, and real-time tracking of needs across diverse populations.
The 2023 Viral Hepatitis Surveillance Status Report (SSR) from HepVu and NASTAD underscores the importance of sustained investment. Drawing on data from 59 U.S. jurisdictions, the report finds that expanded funding has strengthened local surveillance capacity, though progress remains fragile without continued support. The SSR highlights persistent disparities in states’ monitoring capacity, workforce shortages, and uneven access to timely data – all of which directly affect public health preparedness.
Modernized surveillance, including integration with electronic health records and laboratory reporting systems, enhances real-time data sharing among jurisdictions. These advancements enable targeted outreach, close service gaps, and improve measurement across demographic groups. Continued investment in surveillance modernization, as emphasized by the SSR, is crucial to maintaining readiness and strengthening equitable response capacity for hepatitis and other emerging health threats.
4 Ways to Use HepVu
Explore Interactive Maps
View Local Statistics
View local statistics for your state, and download high-impact data visualizations for your work
See the Data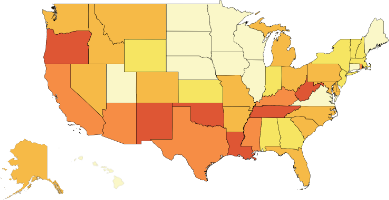
Download Data
See the DataLearn from Experts

October 21, 2020
Thaddeus Pham on Hawaii’s Viral Hepatitis Elimination Strategy
Thaddeus Pham is the Viral Hepatitis Prevention Coordinator for the Hawaii Department of Health’s Harm Reduction Services Branch as well as the co-Founder and co-Director of the Hep Free Hawaii Coalition. Q: Earlier this summer, Hep Free Hawaii, a coalition of over 90 organizations, released its first viral hepatitis elimination strategy for the state of
Read More
December 2, 2019
Vu Q&A: Monica Graybeal on Ending Hep C in Washington State
Dr. Monica Graybeal, PharmD, is a Hepatitis C ambulatory and community pharmacist at Yakima Valley Farm Workers Clinic and an adjunct professor at Washington State University. Q: You’ve been working to diagnose, treat, and care for Hepatitis C patients at the Yakima Valley Farm Workers Clinic in Spokane, Washington, for more than a decade.
Read More
June 5, 2019
Vu Q&A: Shauna Onofrey on Hepatitis C Elimination Efforts in Massachusetts
Shauna Onofrey, MPH is an Epidemiologist at the Massachusetts Department of Public Health Q: You have focused on viral hepatitis in roles with the Centers for Disease Control and Prevention (CDC) to the Massachusetts Department of Public Health (MDPH). How have viral hepatitis and the Hepatitis C epidemic in the U.S. evolved during the course
Read MoreFor More Information
Additional information about viral hepatitis elimination can be found at the following resources.
U.S. Centers for Disease Control and Prevention
The National Viral Hepatitis Progress Report provides information on progress in the implementation of recommended interventions and the impact these interventions are having on the prevention of viral hepatitis transmission, disease, and associated mortality.
Learn MoreU.S. Department of Health and Human Services
A growing number of hepatitis elimination projects are being established across the United States. These projects implement the Viral Hepatitis National Strategic Plan’s call for more coordinated and collaborative efforts aimed at elimination.
Learn MoreWorld Health Organization
The first global health sector strategy on viral hepatitis, a strategy that contributes to the achievement of the 2030 Agenda for Sustainable Development.
Learn MoreThe Task Force for Global Health
The Task Force for Global Health takes on the world’s worst and most intractable diseases to eliminate them or bring them firmly under public health control while strengthening health systems so that countries can protect the health of their populations.
Learn More