HepVu sat down with the team at the Tennessee Department of Health that focuses on perinatal Hepatitis C to discuss their efforts to monitor infants perinatally exposed to Hepatitis C and increase perinatal screening across the state.
- Laura Price, Perinatal Hepatitis C Coordinator, Tennessee Department of Health
- Lindsey Sizemore, MPH, CPH, Viral Hepatitis Program Director at the Tennessee Department of Health
- Heather Wingate, MPH, Viral Hepatitis Epidemiologist at Tennessee Department of Health
Q: Can you tell us how long have you worked for the Tennessee Department of Health and how did you get involved in viral hepatitis surveillance?
Laura Price: I began working with the Tennessee Department of Health in the newborn screening program in October 2015. Before this, I had been a maternal newborn nurse for 24 years. As the Zika virus outbreak emerged in early 2016, I was asked to perform maternal and newborn chart abstractions in a support role.
With the established linkage between Zika and neurologic birth defects, the Tennessee Department of Health formed the Tennessee Birth Defects Surveillance System, which officially launched January 1, 2017. In the spring of 2019, CDC re
leased funding for the Epidemiology and Laboratory Capacity (ELC) grant, which was formally dedicated to Zika surveillance and specified funding towards surveillance and monitoring of other emerging infectious diseases, infants with congenital exposure, and other health preparations.
The Tennessee Department of Health was one of the ELC recipients selected to focus on perinatal Hepatitis C and transitioned into my current role as the perinatal Hepatitis C coordinator in the summer of 2019.
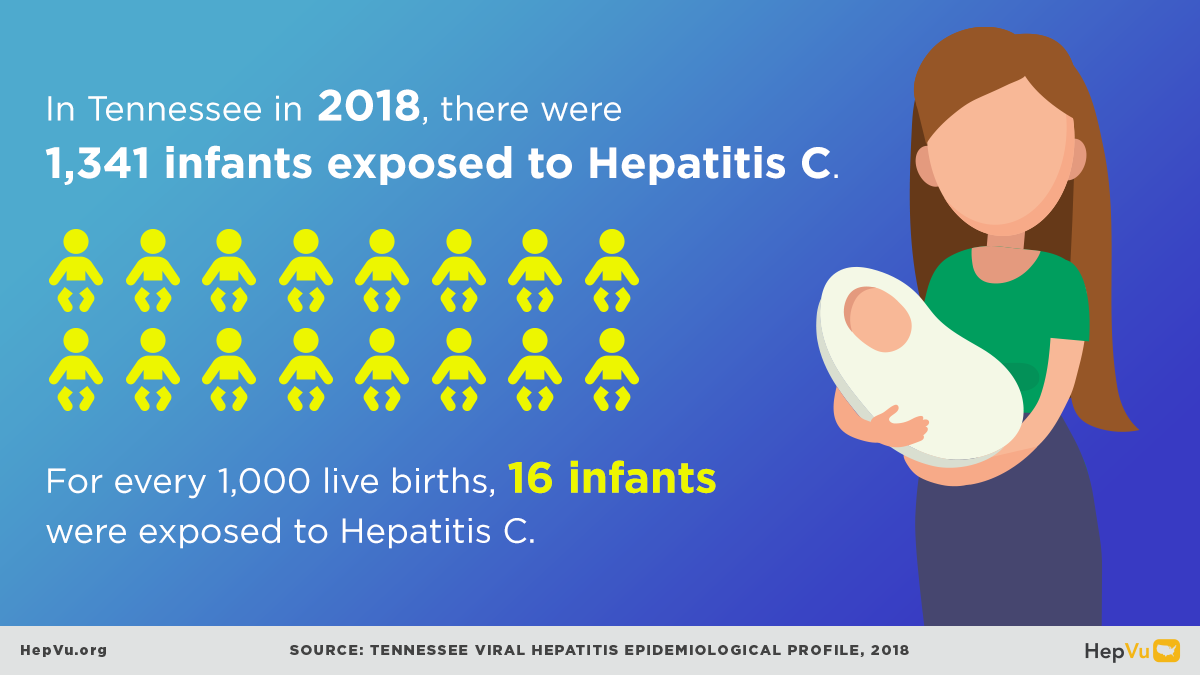
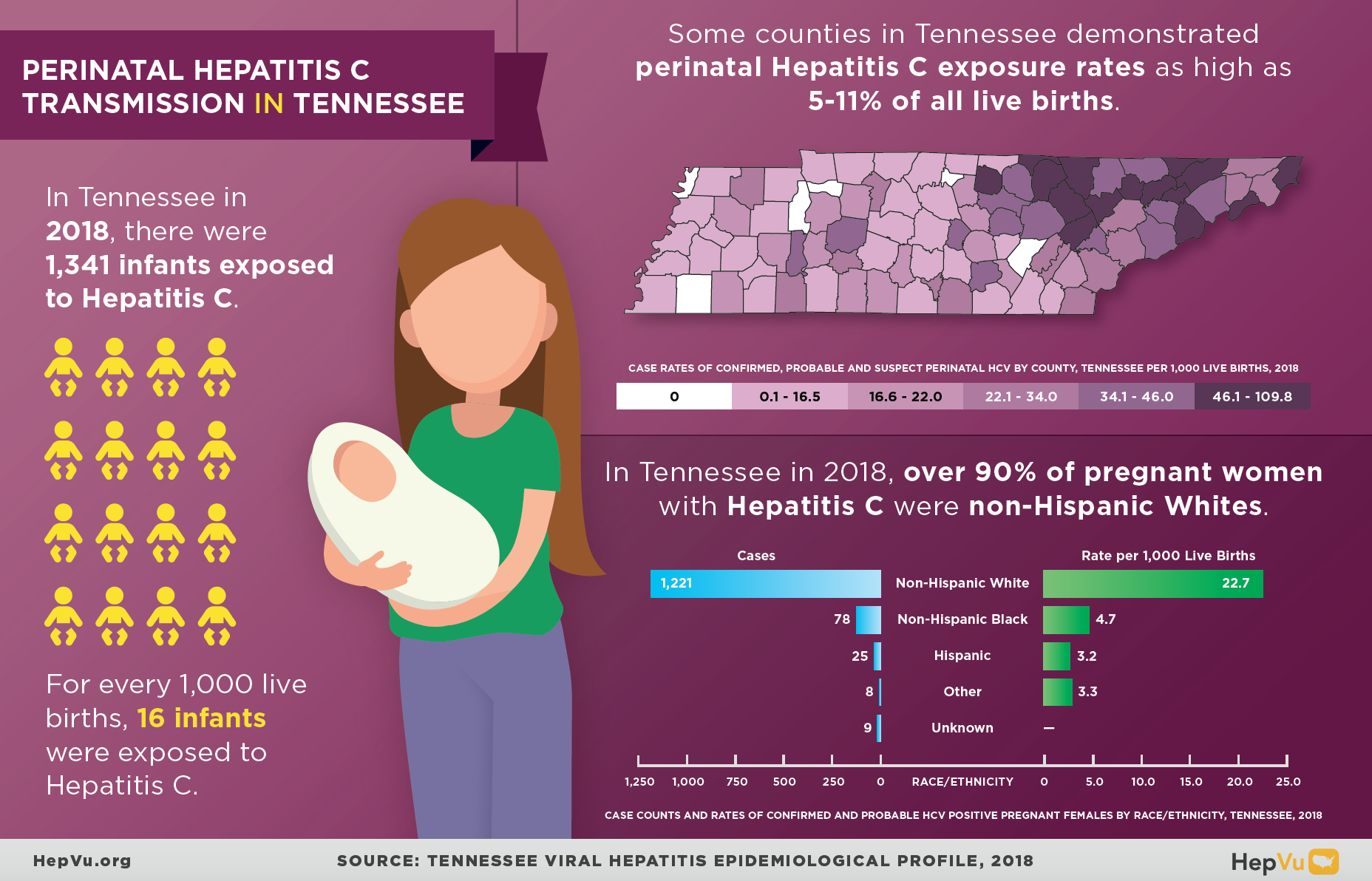
Q: The 2018 Tennessee Viral Hepatitis Epidemiological Profile found that some counties in Tennessee demonstrated perinatal Hepatitis C exposure rates as high as 5-11% of all live births. How do you determine whether infants had been perinatally exposed to Hepatitis C? Can you explain the factors that are contributing to these high rates of exposure?
Heather Wingate: We utilize maternal lab data to determine whether an infant has been perinatally exposed to Hepatitis C. Infants are considered exposed if their mother met one of three criteria:
1. Hepatitis C RNA-positive (viremic) during pregnancy,
2. In the absence of a pregnancy RNA lab, the mother was Hepatitis C RNA-positive (viremic) just before pregnancy, or
3. In the absence of RNA labs, the mother was Hepatitis C antibody positive preceding or during pregnancy.
We have these criteria because we don’t have the confirmatory test, so we decide to rule them in versus ruling them out.
For the second part of your question, while it’s estimated that over 70% of Hepatitis C infections in the U.S. occur among Baby Boomers, the cases reported in Tennessee have a much more bi-modal distribution, with about half of newly reported chronic infections occurring among individuals under the age of 45 – with half of this cohort being female. Additionally, since the routine blood product screening was introduced, mother-to-child transmission of Hepatitis C has become the leading cause of childhood Hepatitis C infection. These increased rates of Hepatitis C among people of reproductive age is mirrored by the increasing rates of injection drug use.
In Tennessee, we see our highest rates of Hepatitis C infection among the white, non-Hispanic rural population, especially in our Appalachian region. Further, with a six percent mother-to-child transmission rate of Hepatitis C, the increasing prevalence of Hepatitis C infection among young women is leading to increasing rates of perinatal Hepatitis C exposure.
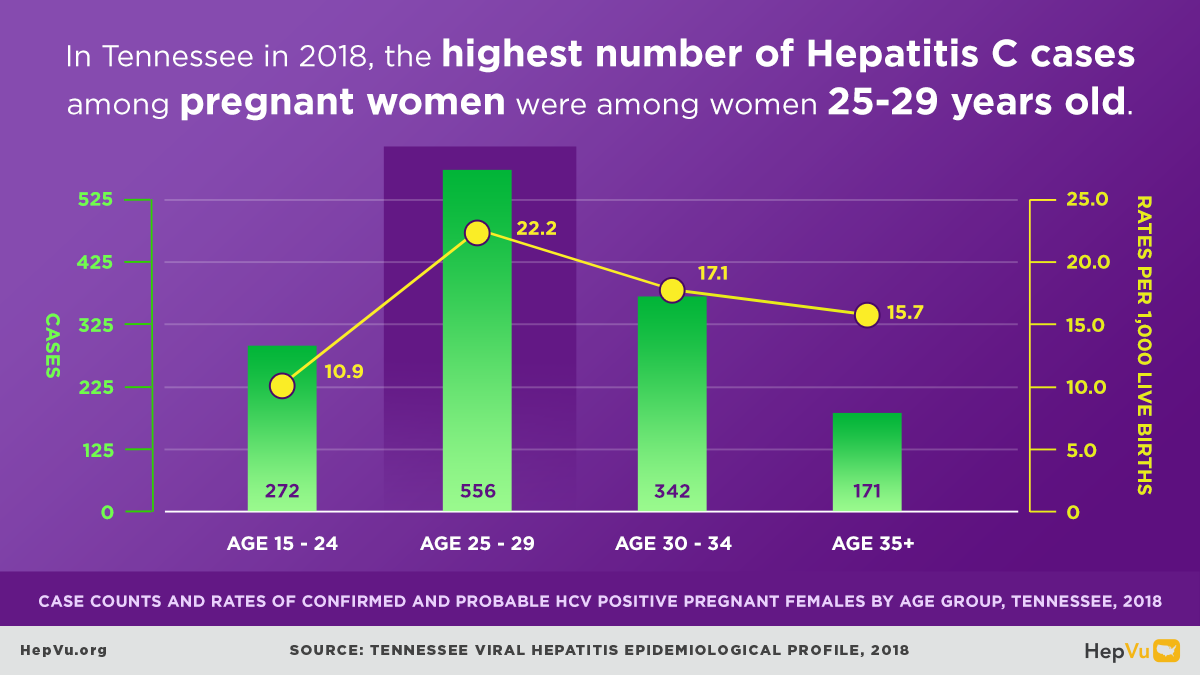
Q: The report also found that in 2018 the highest number of Hepatitis C cases among pregnant women were among young women 25-29 years old. What are some steps local health officials and providers should consider to mitigate the risk of perinatal Hepatitis C transmission?
Lindsey Sizemore: First, we need to ensure that all adults are screened for Hepatitis C infection. The US Preventive Services Task Force recommendation, which was released in March of this year, and the new CDC Hepatitis C recommendations both indicate that all adults should be screened at least once.
We also need to ensure that all pregnant women are screened for Hepatitis C infection. So currently the American Association for the Study of Liver Diseases, the Infectious Diseases Society of America and the US Preventive Services Task Force recommend that pregnant women should be screened, as well as the new CDC Hepatitis C testing recommendations, which now indicate that all pregnant women should be screened during every pregnancy.
Additionally, we need to educate providers and healthcare systems regarding these Hepatitis C testing recommendations. We need to promote the implementation of routine electronic health record prompts in healthcare systems for Hepatitis C testing among all adults and pregnant women. We need to consider introducing legislation requiring every pregnant woman to be tested for Hepatitis C, similar to how we currently test for HIV and syphilis each pregnancy.
I think it is important to link all Hepatitis C positive women to care and treatment. Even though Hepatitis C treatment is not currently recommended during pregnancy, it can be treated postpartum to mitigate the risk in future pregnancies. Finally, we need to ensure access to harm reduction resources for people with a history of drug use.
Q: New Hepatitis C testing guidelines recommend that women are screened for Hepatitis C during each pregnancy. How do you think this will impact rates of perinatal Hep C transmission in Tennessee? What might be some barriers to provider uptake of this recommendation?
Laura Price: I would say that it obviously won’t be impacting the pregnancies at hand. However, I think it will raise awareness among providers and mothers alike. Additionally, the new recommendations will likely lead to an increase in postpartum treatment, which will hopefully decrease perinatal transmission in subsequent pregnancies. This has been a very effective approach in decreasing perinatal HIV in the US when we would anticipate similar things with Hepatitis C over time.
As for changing provider habits, particularly of those providing OB care outside of large academic medical centers, it’s going to take some time and education. But we’re really optimistic about the direction we are headed. If this screening were added as a part of the routine prenatal panel with the assistant laboratories and large academic medical center laboratories, I think it’s doable and will decrease transmission in Tennessee over time.
Q: Hepatitis C infections have been increasing nationwide and there is an ongoing need for expanded, reliable, and consistent viral hepatitis surveillance. What are the most important steps public health officials can take to reach this goal?
Lindsey Sizemore: A major step officials could take would be to increase the funding dedicated to viral hepatitis surveillance. We really need this funding to ensure jurisdictions are ready to do four things:
- Rapidly detect and respond to a viral hepatitis outbreak
- Assess the true burdens and trends of this disease
- Focus limited surveillance resources to have the highest impact
- Monitor progress of ongoing viral hepatitis elimination efforts
Beyond that, we really do need to develop comprehensive chronic Hepatitis C registries and have complete reporting of pertinent laboratory results, including positive and negative Hepatitis C RNA results. As Heather mentioned previously, knowing Hepatitis C RNA results is really important in terms of determining if the woman is viremic during pregnancy.
Locally, health departments need to promote and conduct Hepatitis C testing in high impact settings like, sexually transmitted disease clinics, correctional settings, and syringe service programs. And finally, providers need to ensure exposed infants are appropriately tested for Hepatitis C because that is not something that we’re currently seeing happen in Tennessee.
When Laura Price was conducting navigation, a patient said: “I needed this phone call 9 months ago.” The mothers consistently express gratitude for receiving education about test results and what they actually mean as there is so much misinformation out there. It provides awareness for the mothers as to what their next steps should be for their health, in addition to advocating for Hepatitis C testing for their child(ren).