Hepatitis A
Hepatitis A is a highly contagious liver infection caused by the Hepatitis A virus (HAV).
How Common is Hepatitis A in the U.S.?
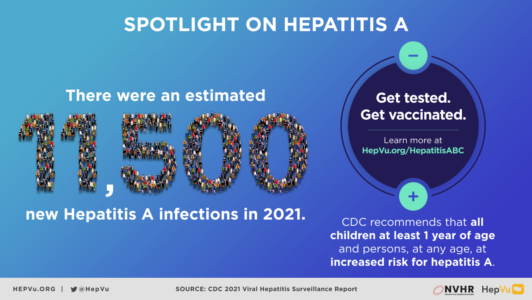
According to the U.S. Centers for Disease Control and Prevention (CDC), during 2021, 50 states reported 5,728 cases, corresponding to 11,500 estimated infections.
During 2021, eight states declared an end to outbreaks. However, the number of cases in 2021 remains 4 times higher than in 2015.
However, Hepatitis A remains a highly undiagnosed disease.
How is Hepatitis A Transmitted?
Hepatitis A is transmitted when a person ingests fecal matter (or stool) from contact with objects, food or drinks contaminated by small undetected amounts of stool from an infected person.
Hepatitis A can also spread from close personal contact with an infected person such as through sex or caring for someone who is ill.
Who is at High Risk of Contracting Hepatitis A?
- All who live in a community with high rates of Hepatitis A
- Travelers to countries where Hepatitis A is common
- Men who have sex with men (MSM)
- People who use drugs, both injection and non-injection
- People with clotting factor disorders, such as hemophilia
- Those with occupational risk (for example, people working with nonhuman primates)
To find out if you are at risk, take the CDC Viral Hepatitis Risk Assessment, and ask your health care providers if you should be vaccinated or tested for Hepatitis A.
What are the Symptoms of Hepatitis A?
Some people contract Hepatitis A and have no symptoms of the disease. However, for those who do experience symptoms, they generally last less than two months and may include symptoms such as nausea, vomiting, abdominal pain, loss of appetite, fever, fatigue, and jaundice. Hepatitis A does not lead to chronic infection. People who are infected with Hepatitis A will eventually clear the virus from their bodies.
How Does a Person Prevent Hepatitis A Infection?
The best way to prevent Hepatitis A infection is to be vaccinated, which will need to be performed more than once in a lifetime for maximum impact. CDC recommends the Hepatitis A vaccine for all children aged 12–23 months, those between 2–18 years of age who have not previously received a vaccine, and adults who may be at risk, including travelers to certain international countries, men who have sex with men (MSM), people with liver disease, and people who are or were recently in jail or prison. Other prevention methods include practicing good hygiene, including washing hands after using the bathroom and changing diapers, and before eating or preparing food. Click here to find out where you can get vaccinated.
Learn more about the efficacy of Hep A vaccinations here.
For more information on Hepatitis A, and to find out if you are at risk for Hepatitis A, visit the CDC’s Hepatitis A Page.
Hepatitis B
Hepatitis B is a liver infection caused by the Hepatitis B virus (HBV).
What is Hepatitis B?
Hepatitis B is an acute illness for some people (defined as the first 6 months following infection), but can often become a long-term, chronic infection. A person’s chances of developing chronic infection are related to the age at which the individual becomes infected. According to the CDC, 90 percent of infants become chronically infected, as opposed to adults who have a 2 to 6 percent chance of developing a chronic infection. Chronic Hepatitis B can lead to serious health issues, such as cirrhosis and liver cancer.
How Common is Hepatitis B in the U.S.?
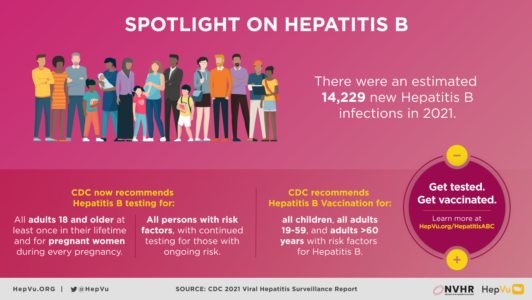
According to CDC, during 2021, 47 states reported 2,045 acute Hepatitis B cases, corresponding to an estimated 13,300 infections and 40 states reported a total of 14,229 newly reported chronic Hepatitis B cases. It is estimated that 862,000 to 2.2 million people in the U.S. were living with the virus in 2021, as people living with the virus are greatly undiagnosed.
After a decade of stable rates, the rate of acute Hepatitis B abruptly decreased in 2020; the rate decreased again by 14% in 2021. This decrease may be related to fewer people seeking healthcare and being tested for Hepatitis B during the COVID-19 pandemic.
How is Hepatitis B Transmitted?
Hepatitis B is transmitted when blood, semen, or other body fluids of an infected person enters the body of an uninfected individual. This can occur through sexual contact, needle sharing, or from mother to child during birth.
Who is at High Risk of Contracting Hepatitis B?
- Infants born to HBV-infected mothers
- Sex partners of HBV-infected persons
- Men who have sex with men (MSM)
- People who inject drugs
- Household contacts or sexual partners of known people with chronic HBV infection
- Health care and public safety workers at risk for occupational exposure to blood or blood-contaminated body fluids
- Hemodialysis patients
To find out if you are at risk, take the CDC Viral Hepatitis Risk Assessment, and ask your health care providers if you should be vaccinated or tested for Hepatitis B.
What are the Symptoms of Hepatitis B?
Symptoms of Hepatitis B vary. Children 5 years and under and newly infected immunosuppressed adults often show no symptoms, while 30 to 50 percent of infected persons ages 5 or older show initial symptoms, including fever, fatigue, nausea, vomiting, abdominal pain, dark urine, clay-colored bowel movements, and jaundice.
How Does a Person Prevent Hepatitis B Infection?
The best way to prevent Hepatitis B infection is to be vaccinated, which occurs in a series of shots over time. Hepatitis B vaccination is recommended for all infants and all children and adolescents younger than 19 years of age who have not been vaccinated; those with sexual partners who have Hepatitis B; those who work in environments where exposure to blood is a risk; and others. Other prevention methods include using sterile tools for body piercings, avoiding needle sharing, and using condoms. Click here to find out where you can get vaccinated.
How is Hepatitis B Treated?
There is no medication available for acute Hepatitis B infection. There are several antiviral medications available for people with chronic infection.
How do Health Care Providers Test for Hepatitis B?
Testing for Hepatitis B involves the measurement of several Hepatitis B virus (HBV)-specific antigens and antibodies. Different serologic “markers” or combinations of markers are used to identify different phases of HBV infection. They can determine whether a patient has acute or chronic HBV infection, is immune to HBV due to prior infection or vaccination, or is susceptible to infection.
Getting tested is the only way to know if you have Hepatitis B. CDC’s Hepatitis B screening recommendations call for:
- People born in countries with moderate or high prevalence of Hepatitis B
- People born in the U.S. not vaccinated as infants whose parents were born in regions with high rates of Hepatitis B
- Men who have sex with men (MSM)
- People who inject drugs
- People living with HIV
- Household and sexual contacts of Hepatitis B infected people
- People requiring immunosuppressive therapy
- People with end-stage renal disease (including hemodialysis patients)
- Blood and tissue donors
- People with elevated alanine aminotransferase levels
- Pregnant women
- Children born to mothers with a Hepatitis B infection
For more information on Hepatitis B, and to find out if you are at risk for Hepatitis B, visit the CDC’s Hepatitis B Page.
Hepatitis C
Hepatitis C is a liver infection caused by the Hepatitis C (HCV) virus.
What is Hep C?
The initial months following infection are referred to as acute Hepatitis C, which can range in severity from few to no symptoms, to a serious condition that requires medical attention. The CDC estimates that approximately 20 percent of people can get rid of the Hepatitis C virus within the first six months following infection without seeking treatment. However, most individuals infected with Hepatitis C go on to develop chronic infection, which may lead to liver disease, liver failure, or liver cancer years or decades later.
How Common is Hepatitis C in the U.S.?
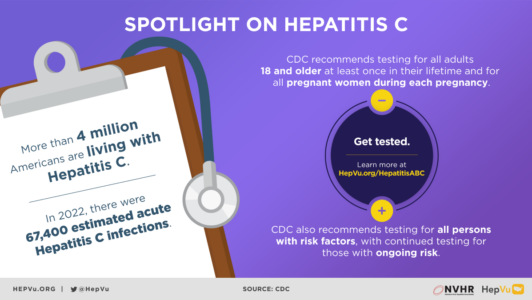
According to CDC, 43 states reported a total of 107,300 newly identified chronic Hepatitis C cases in 2021, corresponding to 39.8 chronic Hepatitis C cases per 100,000 people.
The CDC estimates that there are 4 million individuals in the U.S. living with chronic Hepatitis C.
How is Hepatitis C Transmitted?
Hepatitis C is spread through contact with infected blood. Today, Hepatitis C is most commonly transmitted through the sharing of contaminated needles used to inject drugs. Also, mothers who are infected with Hepatitis C can transmit the infection to their newborn infants. Hepatitis C can also be transmitted through sex, but it is rare. Before 1992, when blood supplies were not universally screened for HCV, Hepatitis C was also spread through blood transfusions and organ transplants. After that, widespread screening of the blood supply in the United States virtually eliminated this source of infection.
What are the Symptoms of Hepatitis C?
When present, Hepatitis C symptoms include fever, fatigue, loss of appetite, nausea, vomiting, dark urine, grey colored stool, and jaundice.
How is Hepatitis C Treated?
There are highly effective treatment options that cure more than 90 percent of people with chronic Hepatitis C. A cure is confirmed after a blood test given 3 months after treatment is completed indicates that the virus is no longer detected in the blood.
How Does a Person Know if they Have Hepatitis C?
Getting tested is the only way to know if you have Hepatitis C. CDC’s Hepatitis C screening recommendations call for:
- One-time screening for all adults 18 years and older.
- Screening of all pregnant women during every pregnancy.
- One‑time Hepatitis C testing regardless of age or setting prevalence among people with increased risk-factors, including those living with HIV, injection drug users, and children born to mothers with a Hepatitis C infection.
- Any person who requests Hepatitis C testing should receive it, regardless of disclosure of risk, because many persons may be reluctant to disclose stigmatizing risks
Why is Testing for Hepatitis C Important?
- Many people don’t have symptoms when they are first infected with Hepatitis C.
- A large proportion (about 8 in 10) of people who do get infected with Hepatitis C will go on to develop chronic Hepatitis C.
- Most people who have chronic Hepatitis C don’t know they have it until they get sick years or decades later.
- When people with chronic Hepatitis C do get sick, most get severe liver disease.
- Chronic Hepatitis C is one of the most common reasons for liver transplants.
- There are now medicines that can cure someone living with chronic Hepatitis C infection.
How do Health Care Providers Test for Hepatitis C?
There are several blood tests used to detect Hepatitis C Virus (HCV) infection. For the HCV antibody test, a positive result means that HCV antibodies were detected in the blood. Once a person has been infected with HCV, the antibodies will stay in the blood system even if the virus is no longer present. Because of this, another test that looks for the presence of the HCV itself in the blood is used – the HCV RNA test. A person who has both a positive HCV antibody test and a positive HCV RNA test is infected with Hepatitis C.
For more information on Hepatitis C, and to find out if you are at risk for Hepatitis C, visit the CDC’s Hepatitis C Page.
Hepatitis D
Hepatitis D is a liver disease caused by the Hepatitis D virus (HDV).
What is Hepatitis D?
Hepatitis D, also known as Hepatitis Delta, is a liver disease caused by the Hepatitis D virus (HDV) according to the Centers for Disease Control and Prevention (CDC). Hepatitis D is known as a “satellite virus,” because it can only infect people who are also infected by the Hepatitis B virus (HBV). Hepatitis D infection can be acute or lead to chronic, long-term illness. The infection can be acquired either simultaneously with Hepatitis B as a coinfection or as a superinfection in people who are already chronically infected with Hepatitis B.
How Common is Hepatitis D in the U.S.?
Hepatitis D infection is uncommon in the United States. Most cases occur among people who migrate or travel to the United States from countries with high rates of endemic Hepatitis D. Because Hepatitis D is not a nationally notifiable condition, the actual number of Hepatitis D cases in the United States is unknown but may be higher than previously suspected.
Where is Hepatitis D most common?
Hepatitis D is most common in Eastern Europe, Southern Europe, the Mediterranean region, the Middle East, West and Central Africa, East Asia, and the Amazon Basin in South America.
How is Hepatitis D Transmitted?
Hepatitis D is mainly transmitted through activities that involve percutaneous (i.e., puncture through the skin) and to a lesser extent through mucosal contact with infectious blood or body fluids (e.g., semen and saliva), including:
- Sex with an infected partner
- Injection-drug use that involves sharing needles, syringes, or drug-preparation equipment
- Birth to an infected mother (rare)
- Contact with blood from or the open sores of an infected person
- Needle sticks or exposures to sharp instruments
- Sharing items (e.g., razors and toothbrushes) with an infected person
Who is at High Risk of Contracting Hepatitis D?
- People chronically infected with Hepatitis B
- Infants born to mothers infected with Hepatitis D
- Sex partners of persons infected with Hepatitis D
- Men who have sex with men
- People who inject drugs
- Household contacts of people with Hepatitis D
- Health care and public safety workers at risk for occupational exposure to blood or blood contaminated body fluids
- Hemodialysis patients
What are the Symptoms of Hepatitis D?
Hepatitis D causes infection and clinical illness only in Hepatitis B-infected people. The signs and symptoms of acute Hepatitis D infection are indistinguishable from those of other types of acute viral hepatitis infections. These include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, clay-colored bowel movements, joint pain, and jaundice. These signs and symptoms typically appear 3–7 weeks after initial infection.
Hepatitis D superinfection can accelerate the progression of chronic Hepatitis B infection.
How Does a Person Prevent Hepatitis D Infection?
Although no vaccine is available for Hepatitis D, Hepatitis B vaccination can protect people from Hepatitis D infection.
How is Hepatitis D Treated?
No treatment is available for Hepatitis D infection specifically. Pegylated interferon alpha has shown some efficacy, but the sustained virologic response rate (a measure of viral clearance) is low (25 percent). New therapies are being evaluated. In cases of fulminant hepatitis and end-stage liver disease, liver transplantation may be considered.
How do Health Care Providers Test for Hepatitis D?
Because cases of Hepatitis D are not clinically distinguishable from other types of acute viral hepatitis, diagnosis can be confirmed only by testing for the presence of antibodies against Hepatitis D and/or Hepatitis D RNA. Hepatitis D infection should be considered in any person with a positive Hepatitis B surface antigen (HBsAG), or current Hepatitis B infection, who has severe symptoms of hepatitis or an acute exacerbation of hepatitis.
Should all people with an active Hepatitis B infection be tested for Hepatitis D?
Recommendations for routine Hepatitis D testing among all persons who have a positive Hepatitis B surface antigen (HBsAG), or current Hepatitis B infection, vary. Currently, the CDC does not recommend this practice and the American Association for the Study of Liver Diseases recommends testing only HBsAG positive persons who are “at high risk.” However, the European Association for the Study of the Liver and the Hepatitis B Foundation both recommend routine testing for Hepatitis D for all people living with Hepatitis B. If there is a high clinical suspicion that a person living with Hepatitis B is also infected with Hepatitis D, testing should be carried out.
